Software Solutions
Our software is customized
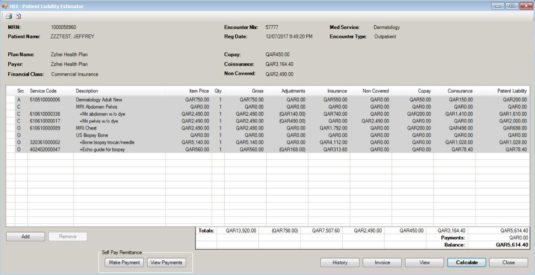
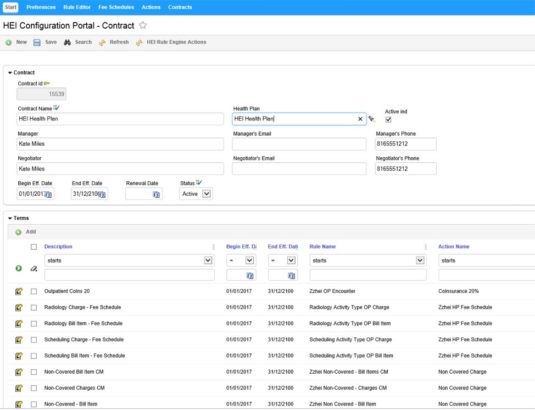
Contract Management
Ability to manage insurance payer and individual health plan contracts in order to accurately predict insurance reimbursement, contractual adjustments and patient liability.
- Calculates patient liabilities, contractual adjustments, DRG (Diagnosis Related Group) Reimbursement and alert prior authorizations
- Web based configuration portal that manages payer contracts, terms, rule and fee schedules
- Flexible rules editor to handle payer requirements
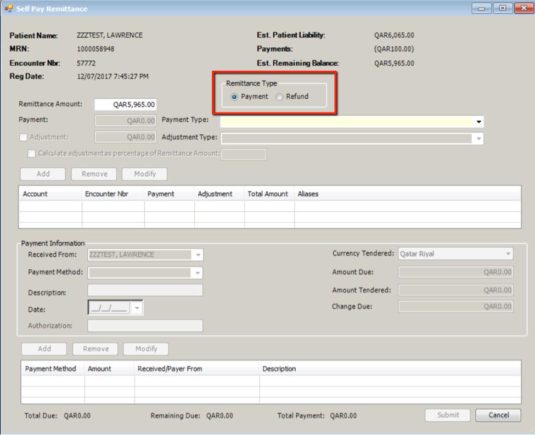
Patient Remittances
Ability to post patient payments and adjustments to billing system which are immediately reflected in estimate and patient account.
- Patient collections prior to services being rendered at time of registration
- Connects to a Point of Sale (POS) device for credit card authorization and payment
- Post patient refunds to billing system
- Print receipt for payments, adjustments, refunds
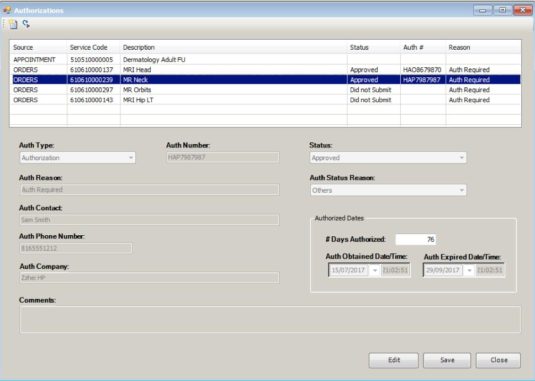
Pre-Authorization
Ability to determine if an insurance payer will cover appointments, procedures or medications prior to services being rendered
- Document and maintain authorization information at the visit or service level
- Automate prior authorization process based on contract terms
- Integrate and post required authorizations on the patient’s clinical record
Eligibility Verification
Ability to perform patient’s insurance coverage verification prior to the procedure or visit.
- Sends insurance verification requests to payers real-time or as batch transactions
- Receive insurance verification responses from payers and automatically populate details to the patient’s record
- Manage pending and denied responses utilizing work queues
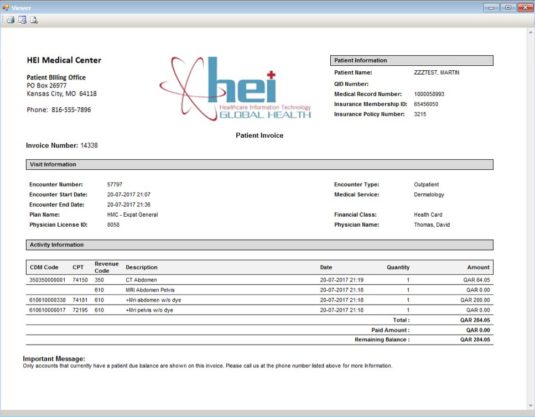
Custom Financial Documents
Ability to produce client defined documents in order to meet the needs of individual organization requirements
- Creation of estimate, claim, invoice and receipt views
- Multi lingual, custom logos, currencies, dates, formats, etc.
Financial Reporting
Financial Reports that enable you to get the financial data necessary to effectively manage accounts based on regional reporting requirements.
- Age Trial Balance (ATB), Discharge Not Final Billed (DNFB), Variance, Cash Reconciliation, Transaction Summary, etc.
- Automated and on demand reporting needs
Claim Scrubber and Population
Ability to build and configure client and payer specific edits based on regional requirements to ensure claim is accurate prior to submission
- Populate custom data elements necessary for governmental and insurance payer requirements
- Alert and manage edit failures through client defined work queues
- Flexible online rule editor to handle complex billing guidelines
Medical Necessity
Ability to evaluate whether a procedure is covered given a specific diagnosis and based on the patient’s health plan
- Check insurance payer content to ensure services will be covered under patient’s insurance
- Evaluate if diagnosis supports the procedure/service at time of physician ordering
Cerner® Integration
HEI Solutions provide an enhanced seamless end user experience by fully integrating our applications directly within the Cerner Architecture.
- HEI solutions are imbedded in Patient Access, Patient Accounting
- All HEI information, configuration and schema are stored within the Cerner Millennium database removing the need for separate third-party applications and interfaces
- All patient, clinical and financial data can easily be reported, evaluated or populated from a single system